There is a lack of consensus on what constitutes the 'ideal' early warning score system. Comparing different systems in clinical use shows variation in which parameters are scored and how those scores are assigned to differing levels of deterioration.
There is however some evidence that certain parameters are better at predicting which patients will die within 24 hours than others. This has led to a call in several countries for the development of a national early warning score that would allow a standardised approach to assessing and responding to deteriorating patients. Early Warning Score VariationsA range of Early Warning Scores have been developed in response to the needs of specific patient types (e.g. This system also demonstrates 'single parameter' triggering whereby an extreme deterioration results in a mandatory MET call which ensures immediate attendance by a Medical Emergency Team to the bedside of the sickest patients.National Early Warning Scoe, UKIn the UK, the Royal College of Physicians has introduced a national early warning score (NEWS) to replace local or regional scores.
The NEWS score is the largest national EWS effort to date, but still remains problematic in the UK due to its lack of universal implementation ability (it has exclusion criteria) and it has yet to have its retrospective validation study published. As medical technology has advanced, so have modern approaches to triage, which are increasingly based on scientific models. The categorizations of the victims are frequently the result of triage scores based on specific physiological assessment findings.
Some models, such as the START model may be algorithm-based. As triage concepts become more sophisticated, triage guidance is also evolving into both software and hardware decision support products for use by caregivers in both hospitals and the field. Triage tags may take a variety of forms. Some countries use a nationally standardized triage tag, while in other countries commercially available triage tags are used, and these will vary by jurisdictional choice.
The most commonly used commercial systems include the METTAG, the SMARTTAG, E/T LIGHT tm and the CRUCIFORM systems. More advanced tagging systems incorporate special markers to indicate whether or not patients have been contaminated by hazardous materials, and also tear off strips for tracking the movement of patients through the process.
Some of these tracking systems are beginning to incorporate the use of handheld computers, and in some cases, bar code scanners. In advanced triage, doctors and specially trained nurses may decide that some seriously injured people should not receive advanced care because they are unlikely to survive. It is used to divert scarce resources away from patients with little chance of survival in order to increase the chances for others with higher likelihoods.The use of advanced triage may become necessary when medical professionals decide that the medical resources available are not sufficient to treat all the people who need help. The treatment being prioritized can include the time spent on medical care, or drugs or other limited resources. This has happened in disasters such as terrorist attacks, mass shootings, volcanic eruptions, earthquakes, tornadoes, thunderstorms, and rail accidents. In these cases some percentage of patients will die regardless of medical care because of the severity of their injuries. Others would live if given immediate medical care, but would die without it.In these extreme situations, any medical care given to people who will die anyway can be considered to be care withdrawn from others who might have survived (or perhaps suffered less severe disability from their injuries) had they been treated instead.
Program Kerja Kepala Sekolah
It becomes the task of the disaster medical authorities to set aside some victims as hopeless, to avoid trying to save one life at the expense of several others.If immediate treatment is successful, the patient may improve (although this may be temporary) and this improvement may allow the patient to be categorized to a lower priority in the short term. Triage should be a continuous process and categories should be checked regularly to ensure that the priority remains correct given the patient's condition. A trauma score is invariably taken when the victim first comes into hospital and subsequent trauma scores are taken to account for any changes in the victim's physiological parameters.
If a record is maintained, the receiving hospital doctor can see a trauma score time series from the start of the incident, which may allow definitive treatment earlier. Usually, triage refers to prioritising admission. A similar process can be applied to discharging patients early when the medical system is stressed. This process has been called 'reverse triage”.
During a 'surge' in demand, such as immediately after a natural disaster, many hospital beds will be occupied by regular non-critical patients. In order to accommodate a greater number of the new critical patients, the existing patients may be triaged, and those who will not need immediate care can be discharged until the surge has dissipated, for example through the establishment of temporary medical facilities in the region.6.
Undertriage and Overtriage● UndertriageUndertriage is underestimating the severity of an illness or injury. An example of this would be categorizing a Priority 1 (Immediate) patient as a Priority 2 (Delayed) or Priority 3 (Minimal). Historically, acceptable undertriage rates have been deemed 5% or less.● OvertriageOvertriage is the overestimating of the severity of an illness or injury. An example of this would be categorizing a Priority 3 (Minimal) patient as a Priority 2 (Delayed) or Priority 1 (Immediate).
Acceptable overtriage rates have been typically up to 50% in an effort to avoid undertriage. Some studies suggest that overtriage is less likely to occur when triaging is performed by hospital medical teams, rather than paramedics or EMTs.
OUTCOMENSThis section is for general concepts in triage-based treatment options and outcomes. For specific triage systems and methods see the sections dedicated to that topic.1.
Palliative careFor those patients that have a poor prognosis and are expected to die regardless of the medical treatment available, palliative care such as painkillers may be given to ease suffering before they die.2. EvacuationIn the field, triage sets priorities for evacuation or relocation to other care facilities.3. Alternative care facilitiesAlternative care facilities are places that are set up for the care of large numbers of patients, or are places that could be so set up. Examples include schools, sports stadiums, and large camps that can be prepared and used for the care, feeding, and holding of large numbers of victims of a mass casualty or other type of event. Such improvised facilities are generally developed in cooperation with the local hospital, which sees them as a strategy for creating surge capacity.

While hospitals remain the preferred destination for all patients, during a mass casualty event such improvised facilities may be required in order to divert low-acuity patients away from hospitals in order to prevent the hospitals becoming overwhelmed. Secondary (in-hospital) triageIn advanced triage systems, secondary triage is typically implemented by emergency nurses, skilled paramedics, or battlefield medical personnel within the emergency departments of hospitals during disasters, injured people are sorted into five categories.Some crippling injuries, even if not life-threatening, may be elevated in priority based on the available capabilities. During peacetime, most amputation injuries may be triaged 'Red' because surgical reattachment must take place within minutes, even though in all probability the person will not die without a thumb or hand. This section is for examples of specific triage systems and methods. For general triage concepts, see the sections for types of triage, treatment options, and outcomes.1. Practical applied triageDuring the early stages of an incident, first responders may be overwhelmed by the scope of patients and injuries. One valuable technique is the Patient Assist Method (PAM).
The responders quickly establish a casualty collection point (CCP) and advise, either by yelling, or over a loudspeaker, that 'anyone requiring assistance should move to the selected area (CCP)'. This does several things at once, it identifies patients that are not so severely injured, that they need immediate help, it physically clears the scene, and provides possible assistants to the responders. As those who can move, do so, the responders then ask, 'anyone who still needs assistance, yell out or raise your hands'; this further identifies patients who are responsive, yet maybe unable to move. Now the responders can rapidly assess the remaining patients who are either expectant, or are in need of immediate aid.
From that point the first responder is quickly able to identify those in need of immediate attention, while not being distracted or overwhelmed by the magnitude of the situation. Using this method assumes the ability to hear. Deaf, partially deaf, or victims of a large blast injury may not be able to hear these instructions. Examples of scoring systems used:A. Triage Revised Trauma Score (TRTS)In Western Europe the Triage Revised Trauma Score (TRTS) is sometimes used and integrated into triage cards.B. Injury Severity Score (ISS)The Injury Severity Score (ISS) is another example of a trauma scoring system.
This assigns a score from 0 to 75 based on severity of injury to the human body divided into three categories:A. (face/ neck/ head),B. (thorax/ abdomen),C. (extremities/ external/ skin).Each category is scored from 0 to 5 using the Abbreviated Injury Scale, from uninjured to critically injured, which is then squared and summed to create the ISS.
A score of 6, for 'unsurvivable', can also be used for any of the three categories, and automatically sets the score to 75 regardless of other scores. Depending on the triage situation, this may indicate either that the patient is a first priority for care, or that he or she will not receive care owing to the need to conserve care for more likely survivors. (Simple Triage and Rapid Treatment) is a simple triage system that can be performed by lightly trained lay and emergency personnel in emergencies.
It is not intended to supersede or instruct medical personnel or techniques. It has been taught to California emergency workers for use inearthquakes. It was developed at Hoag Hospital in Newport Beach, California for use by emergency services.
It has been field-proven in mass casualty incidents such astrain wrecks and bus accidents, though it was developed for use by community emergency response teams (CERTs) and firefighters after earth quakes.Triage separates the injured into four groups:. The expectant who are beyond help. The injured who can be helped byimmediate transportation. The injured whose transport can be delayed. Those with minor injuries, who need help less urgentlyTriage also sets priorities for evacuation and transport as follows:. Deceased are left where they fell. These people are not breathing and an effort to reposition their airway has been unsuccessful.
Immediate or Priority 1 (red) evacuation by MEDEVAC if available or ambulance as they need advanced medical care at once or within 1 hour. These people are in critical condition and would die without immediate assistance. Delayed or Priority 2 (yellow) can have their medical evacuation delayed until allimmediate persons have been transported. These people are in stable condition but require medical assistance. Minor or Priority 3 (green) are not evacuated until all immediate and delayedpersons have been evacuated. These will not need advanced medical care for at least several hours.
Continue to re-triage in case their condition worsens. These people are able to walk, and may only require bandages and antiseptic. This triage position is often done by a hospitalist. A major factor contributing to the triage decision is available hospital bed space. The triage hospitalist must determine, in conjunction with a hospital's 'bed control' and admitting team, what beds are available for optimal utilization of resources in order to provide safe care to all patients. A typical surgical team will have their own system of triage for trauma and general surgery patients.
This is also true for neurology and neurosurgical services. The overall goal of triage, in this system, is to both determine if a patient is appropriate for a given level of care and to ensure that hospital resources are utilized effectively. In an advanced triage process injured people are sorted into categories.
In the mid-1980s, The Victoria General Hospital, in Halifax, Nova Scotia, Canada, introduced paramedic triage in its Emergency Department. Unlike all other centres in North America that employ physician and primarily nurse triage models, this hospital began the practice of employing Primary Care level paramedics to perform triage upon entry to the Emergency Department. In 1997, following the amalgamation of two of the city's largest hospitals, the Emergency Department at the Victoria General closed.
The paramedic triage system was moved to the city's only remaining adult emergency department, located at the New Halifax Infirmary. In 2006, a triage protocol on whom to exclude from treatment during a flu pandemic was written by a team of critical-care doctors at the behest of the Ontario government. For routine emergencies, many locales in Canada now employ the Canadian Triage and Acuity Scale (CTAS) for all incoming patients. The system categorizes patients by both injury and physiological findings, and ranks them by severity from 1–5 (1 being highest). The model is used by both paramedics and E/R nurses, and also for pre-arrival notifications in some cases. The model provides a common frame of reference for both nurses and paramedics, although the two groups do not always agree on scoring. It also provides a method, in some communities, for benchmarking the accuracy of pre-triage of calls using AMPDS (What percentage of emergency calls have return priorities of CTAS 1,2,3, etc.) and these findings are reported as part of a municipal performance benchmarking initiative in Ontario.
Curiously enough the model is not currently used for mass casualty triage, and is replaced by the START protocol and METTAG triage tags. In the UK, the commonly used triage system is the Smart Incident Command System, taught on the MIMMS (Major Incident Medical Management (and) Support) training program. The UK Armed Forces use this system on operations.
This grades casualties from Priority 1 (needs immediate treatment) to Priority 3 (can wait for delayed treatment). Afterwards, casualties are given an evacuation priority based on need:Urgent. Evacuation is required within two hours to save life or limb.Priority. Evacuation is necessary within four hours or the casualty will deteriorate to 'Urgent'.Routine. Evacuate within 24 hours to complete treatment.In a 'naval combat situation', the triage officer must weigh the tactical situation with supplies on hand and the realistic capacity of the medical personnel. This process can be ever-changing, dependent upon the situation and must attempt to do the maximum good for the maximum number of casualties.Field assessments are made by two methods. GermanyPreliminary assessment of injuries is usually done by the first ambulance crew on scene, with this role being assumed by the first doctor arriving at the scene.
As a rule, there will be no cardiopulmonary resuscitation, so patients who do not breathe on their own or develop circulation after their airways are cleared will be tagged 'deceased'. Also, not every major injury automatically qualifies for a red tag. A patient with a traumatic amputation of the forearm might just be tagged yellow, have the bleeding stopped, and then be sent to a hospital when possible. After the preliminary assessment, a more specific and definite triage will follow, as soon as patients are brought to a field treatment facility.
There, they will be disrobed and fully examined by an emergency physician. This will take approximately 90 seconds per patient.The German triage system also uses four, sometimes five colour codes to denote the urgency of treatment.
Typically, every ambulance is equipped with a folder or bag with coloured ribbons or triage tags.The urgency is denoted as follows. LIMITATIONT OF CURRENT PRACTICENotions of mass casualty triage as an efficient rationing process of determining priority based upon injury severity are not supported by research, evaluation and testing of current triage practices, which lack scientific and methodological bases. START and START-like (START) triage that use color-coded categories to prioritize provide poor assessments of injury severity and then leave it to providers to subjectively order and allocate resources within flawed categories. Some of these limitations include:. Lacking the clear goal of maximizing the number of lives saved, as well as the focus, design and objective methodology to accomplish that goal (a protocol of taking the worst Immediate – lowest chances for survival – first can be statistically invalid and dangerous).
Using trauma measures that are problematic (e.g., capillary refill) and grouping into broad color-coded categories that are not in accordance with injury severities, medical evidence and needs. Research indicates there are wide ranges and overlaps of survival probabilities of the Immediate and Delayed categories, and other START limitations. The same physiologic measures can have markedly different survival probabilities for blunt and penetrating injuries.
For example, a START Delayed (second priority) can have a survival probability of 63% for blunt trauma and a survival probability of 32% for penetrating trauma with the same physiological measures – both with expected rapid deterioration, while a START Immediate (first priority) can have survival probabilities that extend to above 95% with expected slow deterioration. Age categories exacerbate this. For example, a geriatric patient with a penetrating injury in the Delayed category can have an 8% survival probability, and a pediatric patient in the Immediate category can have a 98% survival probability. Issues with the other START categories have also been noted. In this context, color-coded tagging accuracy metrics are not scientifically meaningful.
ETHICAL IMPLICATIONBecause treatment is intentionally delayed or withheld from patients, advanced triage has ethical implications.Bioethical concerns have historically played an important role in triage decisions, such as the allocation of iron lungs during the polio epidemics of the 1940s and of dialysis machines during the 1960s.As many health care systems in the developed world continue to plan for an expected influenza pandemic, bioethical issues regarding the triage of patients and the rationing of care continue to evolve. Similar issues may occur for paramedics in the field in the earliest stages of mass casualty incidents when large numbers of potentially serious or critical patients may be combined with extremely limited staffing and treatment resources.Research continues into alternative care, and various centers propose medical decision-support models for such situations.
Some of these models are purely ethical in origin, while others attempt to use other forms of clinical classification of patient condition as a method of standardized triage. These three scores (Glasgow Coma Scale, Systolic Blood Pressure, Respiratory Rate) are then used to take the weighted sum by RTS = 0.9368 GCS + 0.7326 SBP + 0.2908 RR.
Values for the RTS are in the range 0 to 7.8408. The RTS is heavily weighted towards the Glasgow Coma Scale to compensate for major head injury without multisystem injury or major physiological changes. A threshold of RTS. Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ (September 1981).
'Trauma score'. 9 (9): 672–6.doi:10.106-19815.PMID 7273818. Taber, Clarence Wilbur; Venes, Donald (2009).
Taber's cyclopedic medical dictionary. F a Davis Co. ISBN 0-8036-1559-0. Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME (May 1989). 'A revision of the Trauma Score'.
The Journal of Trauma. 29 (5): 623–9.doi:10.103-19897.PMID 2657085.
REFERENCES. Rancho Los Amigos National Rehabilitation Center. (1 March 2011). The Rancho Levels of Cognitive Functioning. Retrieved May 15, 2011, from Fulk, G. Traumatic Brain Injury. O’Sullivan & T.
Schmitz (Eds.), Physical Rehabilitation (5th ed., pp. Philadelphia, PA: F. Davis Company. Gouvier, W.
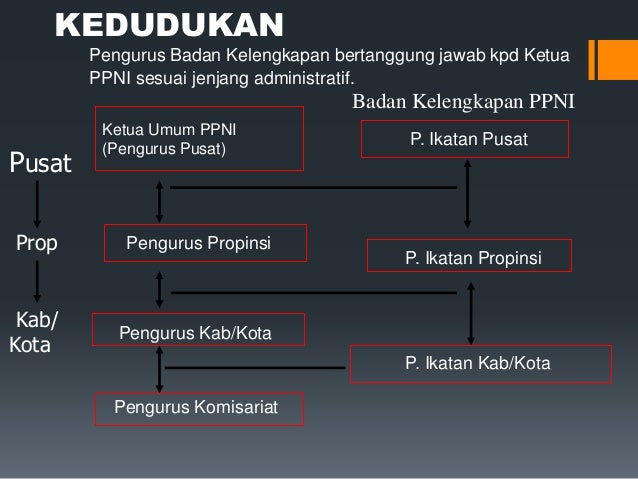
Ppni
D., Blanton, P. D., LaPorte, K.
K., & Nepomuceno, C. Reliability and validity of the Disability Rating Scale and the Levels of Cognitive Functioning Scale in monitoring recovery from severe head injury.Archives of Physical Medicine and Rehabilitation, 68(2), 94-97. VERBAL: The patient makes some kind of response when you talk to them, which could be in any of the three component measures of eyes, voice or motor - e.g. Patient's eyes open on being asked 'Are you OK?' The response could be as little as a grunt, moan, or slight move of a limb when prompted by the voice of the rescuer.
PAIN: The patient makes a response on any of the three component measures on the application of pain stimulus, such as a central pain stimulus like a sternal rub or a peripheral stimulus such as squeezing the fingers. A patient with some level of consciousness (a fully conscious patient would not require a pain stimulus) may respond by using their voice, moving their eyes, or moving part of their body (includingabnormal posturing). UNRESPONSIVE: Sometimes seen noted as 'Unconscious', this outcome is recorded if the patient does not give any eye, voice or motor response to voice or pain. Kelly, CA; Upex A; Bateman DN. (February 2005). 'Comparison of consciousness level assessment in the poisoned patient using the alert/ verbal/ painful/ unresponsive scale and the Glasgow Coma Scale'. Annals of Emergency Medicine.
44 (2): 108–113.doi:10.1016/j.annemergmed.2004.03.028. a b McNarry, AF; Bateman, DN (January 2004). 'Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma scale'.
59 (1): 34–7.doi:10.1111/j.1365-2044.2004.03526.x.PMID 14687096. The Paediatric Glasgow Coma Scale (BrE) (also known as Pediatric Glasgow Coma Score (AmE) or simply PGCS) is the equivalent of the Glasgow Coma Scale (GCS) used to assess the level of consciousness of child patients. As many of the assessments for an adult patient would not be appropriate for infants, the Glascow Coma Scale was modified slightly to form the PGCS. As with the GCS, the PGCS comprises three tests: eye,verbal and motor responses. The three values separately as well as their sum are considered. The lowest possible PGCS (the sum) is 3 (deep coma or death) whilst the highest is 15 (fully awake and aware person).
The pediatric GCS is commonly used in emergency medical services.
